Coronavirus (COVID-19) Update: Testing copayment waiver: Retroactive to March 18, 2020, TRICARE will waive copayments/cost-shares for medically necessary COVID-19 diagnostic and antibody testing and related services, and office visits, urgent care or emergency room visits during which tests are ordered or administered. COVID-19 diagnostic and antibody tests must meet Families First Coronavirus. . $25 office visit copay. 20% coinsurance all other charges (even if related to office visit) Not covered: Deductible doesn’t apply to copay for office visit charge only. Copay doesn’t count toward deductible. Deductible and coinsurance apply to all other in-network charges.
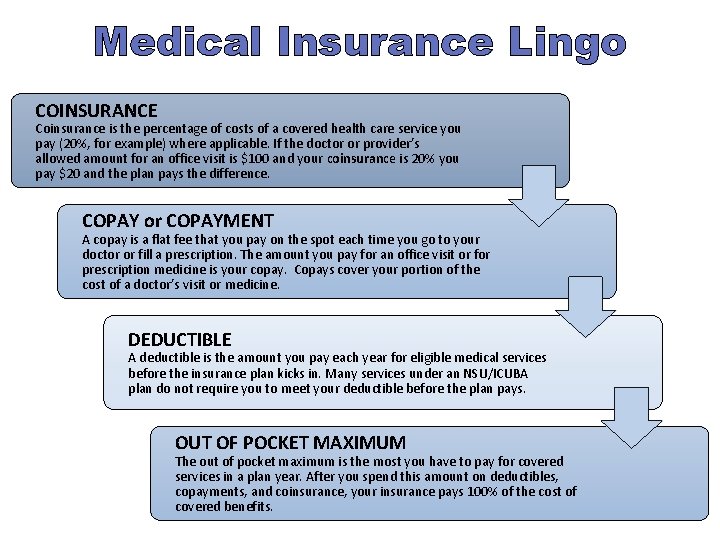
A copay is a fixed amount you pay for a health care service, usually when you receive the service. The amount can vary by the type of service. How it works: Your plan determines what your copay is for different types of services, and when you have one. You may have a copay before you’ve finished paying toward your deductible. Doctor's Office Visits In-Network: Primary care physician visit: $15 Copay. You pay $0 copay for an office visit with your primary care provider within 30-days of an inpatient hospital stay. Primary Care Physician is defined as Family Practitioners, General Practitioners, Internal.
Cite thisWhat you need to know about mental health coverage
When it comes to our well-being, mental health is just as important as physical health. Unfortunately, insurers haven’t always seen it that way. In the past, many health insurance companies provided better coverage for physical illness than they did for mental health disorders.
A law passed in 2008, the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (also known as the mental health parity law or federal parity law) requires coverage of services for mental health, behavioral health and substance-use disorders to be comparable to physical health coverage. Yet many people still aren’t aware that the law exists or how it affects them. In fact, a 2014 APA survey found that more than 90 percent of Americans were unfamiliar with the mental health parity law.
This guide helps you learn what you need to know about mental health coverage under the mental health parity law.
What does the law do?
The federal parity law requires insurance companies to treat mental and behavioral health and substance use disorder coverage equal to (or better than) medical/surgical coverage. That means that insurers must treat financial requirements equally. For example, an insurance company can’t charge a $40 copay for office visits to a mental health professional such as a psychologist if it only charges a $20 copay for most medical/surgical office visits.
The parity law also covers non-financial treatment limits. For instance, limits on the number of mental health visits allowed in a year were once common. The law has essentially eliminated such annual limits. However, it does not prohibit the insurance company from implementing limits related to “medical necessity.”
What health plans does the law affect?
The federal parity law generally applies to the following types of health insurance:
- Employer-sponsored health coverage, for companies with 50 or more employees
- Coverage purchased through health insurance exchanges that were created under the health care reform law also known as the Affordable Care Act or “Obamacare”
- Children’s Health Insurance Program (CHIP)
- Most Medicaid programs. (Requirements may vary from program to program. Contact your state Medicaid director if you are not sure whether the federal parity law applies to your Medicaid program.)
Some other government plans and programs remain exempt from the parity law. Medicare, unlike Medicaid, for instance, is not subject to the federal parity law. And some state government employee plans (including ones that cover teachers and employees of state universities, for instance) may opt out of the parity requirements.
How do I know if my health insurance plan provides mental health coverage?
Check your description of plan benefits—it should include information on behavioral health services or coverage for mental health and substance-use disorders. If you still aren’t sure, ask your human resources representative or contact your insurance company directly.
My insurance plan doesn’t have mental health benefits. Is that a violation of the parity law?
The parity law does not require insurers to provide mental health benefits—rather, the law states that if mental health benefits are offered, they can’t have more restrictive requirements than those that apply to physical health benefits. Fortunately, the vast majority of large group plans already provided mental health benefits before the parity law took effect. In addition, the Affordable Care Act requires that plans offered through the health insurance exchanges cover services for mental health and substance-use disorders.
Are all mental health diagnoses covered by the parity law?
Unlike some state parity laws, the federal parity law applies to all mental health and substance-use disorder diagnoses covered by a health plan. However, a health plan is allowed to specifically exclude certain diagnoses—whether those diagnoses are considered to be in the physical/medical realm or behavioral/mental health. Any exclusions should be made clear to you in your plan’s description of mental health benefits. If you are uncertain ask your insurance company.
My insurance company won’t reimburse me for a therapy visit because I haven’t met my deductible. Is that a violation of the parity law?
A deductible is the overall amount that you must pay out of your own pocket per year before your health insurance makes any payments. Depending on your plan’s deductible, for instance, you may have to pay $500, or even $5,000, out of pocket before your insurance company will pay any claims.
Prior to the parity law, many insurance plans required patients to meet different and often higher deductibles for mental health services than for medical services. As a result of the law, a single deductible now applies to both mental health treatment and medical services. In some cases, your plan may pay for mental health treatment after you have paid part of your deductible but not cover physical health treatment until you have reached the full deductible.
My copay is $20 when I see my psychologist, but only $10 when I visit my primary care physician. Isn’t that against the law?
Not necessarily. The parity law requires copays for mental health services to be equal to or less than the copay for most—not all—medical/surgical services. In this case, for example, it’s acceptable to pay a $20 copay for a mental health visit and a $10 copay for a primary care visit, as long as your copay is $20 or more for most of the medical/surgical services covered by your plan.
My insurance company has only approved a certain number of therapy sessions to treat my disorder. Is this a violation of the parity law?
The parity law prevents insurers from putting a firm annual limit on the number of mental health sessions that are covered. However, insurance companies can still manage your care. Your plan may say, for example, that after 10 or 20 appointments with a psychologist, they will evaluate your case to determine whether additional treatment is “medically necessary” according to their criteria. This kind of management is generally permissible under the parity law if the company uses the same standards for determining mental health coverage as they use to decide what medical services to cover. But if the company terminates or reduces care much sooner than your psychologist thinks is appropriate, that could indicate a possible violation of the parity law.
My mental health provider won’t accept my insurance, even though I have mental health coverage. Why not?
Psychologists and other mental health providers can choose whether or not to accept insurance. Unfortunately, many insurance companies have not increased the reimbursement rate for psychologists in 10 or even 20 years despite the rising administrative costs of running a practice. Other companies have recently cut their reimbursement rates. As a result, some plans have trouble attracting mental health professionals to participate in their networks.
If your options seem limited and your insurance is provided through your employer, you might consider discussing your concerns with your human resources representative. He or she may take that into consideration when negotiating your company’s plan with insurance companies in the future.
My insurance covers out of network providers. What do I need to do get reimbursed for psychotherapy services?

If your health plan covers out of network providers for mental health services and you are seeing a mental health provider who does not accept your insurance, complete your insurance claim form and submit it along with the mental health provider’s invoice to get reimbursed. If you are unsure about your health plan’s claim procedures for out of network providers, contact your insurance company.
Who should I talk to if I think my insurance company is violating the parity law?
If you have concerns that your plan isn’t complying with the parity law, ask your human resources department for a summary of benefits to better understand your coverage, or contact your insurance company directly. Your human resource department can provide you with information about your coverage and may be able to put you in touch with a health care advocate who can assist in making an appeal. If other employees are having similar issues, your HR department may wish to keep track of the problems and work with the insurance company to ensure that benefits are meeting employee needs.
If you do not have an HR department or if your insurance is not provided by your employer, you may wish to speak with the insurance company directly. To reach out to your insurance company, check for a customer service number on the back of your insurance card. If you obtained your insurance through an insurance exchange, you may be able to get help from your state insurance commissioner.
If you still have unanswered questions or wish to file a parity complaint, visit the U.S. Department of Health and Human Services to find the appropriate agency to assist. You can also call the EBSA toll-free consumer assistance line at (866) 444-3272. The federal government’s Consumer Assistance Program website is another good resource.
You may also visit the Parity Track website for information about mental health parity or links to state agencies, as well as other valuable resources. Note that this website offers you the chance to submit a complaint with them about your experience. Registering a complaint with Parity Track is not a substitute for filing an appeal or filing a complaint with a governmental agency. This information is used to influence policy.
Using your mental health coverage
Check with your human resources department or insurance company for specific details about your coverage. Here are some important points to consider:
- Check to see whether your coverage uses provider networks. Typically, patients are required to pay more out-of-pocket costs when visiting an out-of-network provider. Call your insurance company or visit the company’s website for a list of in-network providers.
- Ask about copayments. A copay is a charge that your insurance company requires you to pay out of pocket for a specific service. For instance, you may have a $20 copay for each office visit. In the past, copays for mental health visits may have been greater than those for most medical visits. That should no longer be the case for insurance plans subject to the parity law.
- Ask about your deductible. A deductible is the amount that you must pay out-of-pocket before your health insurance makes any payments. Depending on your deductible, for instance, you may have to pay $500 or even $5,000 out-of-pocket before your insurance company will begin making payments on claims. As a result of the parity law, your deductible should apply to both mental and physical health coverage.
- Talk to your provider. When you call to schedule an appointment with a mental health provider, ask if he or she accepts your insurance. Also ask whether he or she will bill your insurance company directly and you just provide a copayment, or if you have to pay in full and then submit the claim to your insurance company for reimbursement. If your provider does not accept insurance, ask about his or her payment policy.
The full text of articles from APA Help Center may be reproduced and distributed for noncommercial purposes with credit given to the American Psychological Association. Any electronic reproductions must link to the original article on the APA Help Center. Any exceptions to this, including excerpting, paraphrasing or reproduction in a commercial work, must be presented in writing to the APA. Images from the APA Help Center may not be reproduced.

Coronavirus (COVID-19) Update:
Providers are expected to refund cost-sharing amounts to beneficiaries as appropriate. |
- TRICARE Select, TRICARE Young Adult Select, TRICARE Reserve Select, and TRICARE Retired Reserve annual deductibles apply.
- TRICARE Young Adult costs are based on the sponsor's status.
- TRICARE Prime and TRICARE Young Adult Prime retirees have a separate copayment for allergy shots performed on a different day than the office visit, or performed by a different provider, such as an independent laboratory or radiology facility (even if performed on the same day as the related office visit).
- Transitional Assistance Management Program (TAMP) beneficiaries (service members and their family members) follow the active duty family member copayment/cost-share information, based on the TRICARE plan type.
A beneficiary's cost is determined by the sponsor's initial enlistment or appointment date:
- Group A: Sponsor's enlistment or appointment date occurred prior to Jan. 1, 2018.
- Group B: Sponsor's enlistment or appointment date occurred on or after Jan. 1, 2018.
TRICARE Prime and TRICARE Prime Remote (not including TRICARE Young Adult)
| Service | Active Duty Family Members | Retirees and Their Family Members |
|---|---|---|
| Primary Care Outpatient Office Visits | Group A: $0 Group B: $0 | Group A: $21 Group B: $21 |
Specialty Care Outpatient (this includes physical, occupational | Group A: $0 Group B: $0 | Group A: $31 Group B: $31 |
TRICARE Select (not including TRICARE Young Adult)
| Service | Active Duty Family Members | Retirees and Their Family Members |
|---|---|---|
| Primary Care Outpatient Office Visits | Group A: Network Provider: $22 Group B: Network Provider: $15 | Group A: Network Provider: $30 Group B: Network Provider: $26 |
Specialty Care Outpatient (this includes physical, occupational | Group A: Network Provider: $34 Group B: Network Provider: $26 | Group A: Network Provider: $46 Group B: Network Provider: $42 |
Doctor Office Visit Charges
TRICARE Reserve Select (TRS) and TRICARE Retired Reserve (TRR)
| Service | TRS | TRR |
|---|---|---|
| Primary Care Outpatient Office Visits | Network Provider: $15 Non-Network Provider: 20% | Network Provider: $26 Non-Network Provider: 25% |
Specialty Care Outpatient (this includes physical, occupational | Network Provider: $26 Non-Network Provider: 20% | Network Provider: $42 Non-Network Provider: 25% |
TRICARE Young Adult (TYA)
Medicare Part B Office Visit Copay
Copayments Health Insurance
| Service | TYA Prime | TYA Select | ||
|---|---|---|---|---|
| Active Duty Family Members | Retiree Family Members | Active Duty Family Members | Retiree Family Members | |
| Primary Care Outpatient Office Visits | $0 | $21 | Network Provider: $15 Non-Network Provider: 20% | Network Provider: $26 Non-Network Provider: 25% |
Specialty Care Outpatient Office Visits (this includes physical, | $0 | $31 | Network Provider: $26 Non-Network Provider: 20% | Network Provider: $42 Non-Network Provider: 25% |
